New India Health Insurance
Founded in 1919 by Sir Dorabji Tata, New India Assurance Company was a...Read More
3000+
Network hospitals
90.73%
Claim settlement ratio
Up to2 Crore
Sum insured
11
No. of Plans
1.8
Solvency Ratio
1800+
Pan India Presence
11+ Years
IRDAI Approved
5M+
Quotes Generated
100K+
Happy Customers
PolicyX is one of India's leading digital insurance platform
11+ Years
IRDAI Approved
5M+
Quotes Generated
100K+
Happy Customers
PolicyX is one of India's leading digital insurance platform
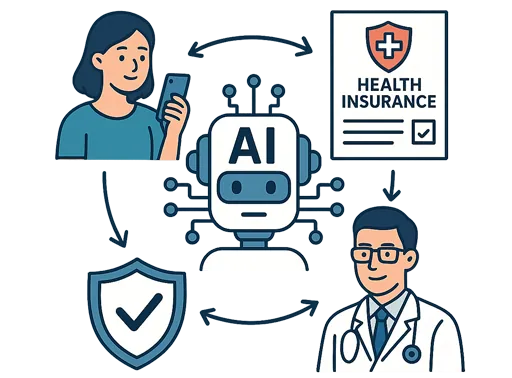
PolicyX Exclusive Benefits
No Spam
No Gimmicks

Personalised
Insurance Advice
24×7
Claim Assistance













































1155-1723614429.webp)









Do you have any thoughts you’d like to share?