Bajaj Allianz’s Health Infinity Policy comes with new ...Read More
18400+
Network hospitals
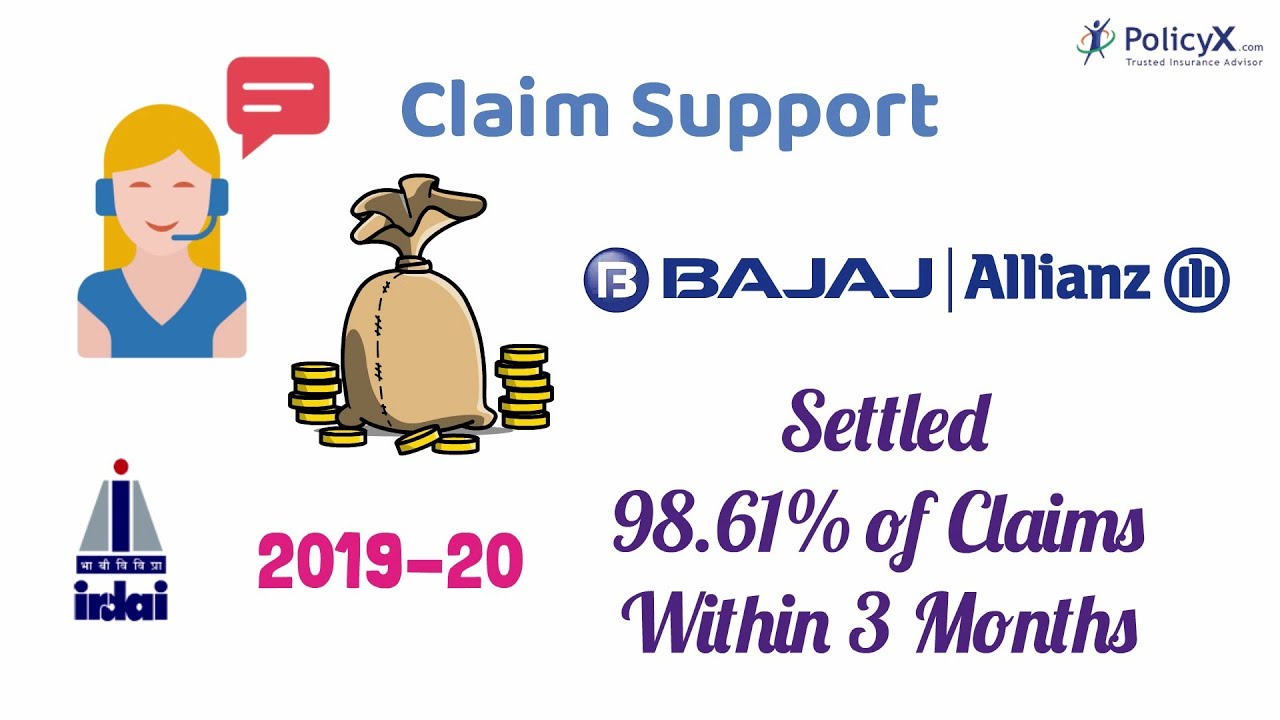
99.23%
Claim settlement ratio
Up to 25 Cr
Sum insured
1
No. of Plans
3.49
Solvency Ratio
1100+
Pan India Presence
11+ Years
IRDAI Approved
5M+
Quotes Generated
100K+
Happy Customers
PolicyX is one of India's leading digital insurance platform
11+ Years
IRDAI Approved
5M+
Quotes Generated
100K+
Happy Customers
PolicyX is one of India's leading digital insurance platform
PolicyX Exclusive Benefits
No Spam
No Gimmicks

Personalised
Insurance Advice
24×7
Claim Assistance














































Do you have any thoughts you’d like to share?